Navigating the Complexities of Medical Claims Management and Practice Management in Healthcare

In the ever-evolving landscape of healthcare, efficient management of medical claims management and practice operations is crucial for ensuring the financial viability and operational success of healthcare providers. Both medical claims management and practice management play vital roles in the smooth functioning of healthcare practices, impacting everything from patient satisfaction to financial health. This article delves into the key aspects of medical claims management and practice management, providing insights into best practices, challenges, and emerging trends.
Key Components of Medical Claims Management:
- Claim Submission: Accurate and timely submission of claims to insurance companies is the first step in the process. This involves coding diagnoses and procedures correctly, ensuring all required documentation is included, and adhering to payer-specific guidelines.
- Claims Processing: Once submitted, claims are reviewed by the insurance payer for accuracy and completeness. This stage may involve communication between the healthcare provider and the payer to resolve any discrepancies or additional information requests.
- Denials and Appeals: Claims may be denied or rejected due to errors, missing information, or policy issues. Effective healthcare claims management includes identifying the reasons for denials, rectifying the issues, and resubmitting or appealing claims as necessary.
The Role of Practice Management
Practice management encompasses the broader scope of administrative and operational tasks involved in running a healthcare practice. It involves the day-to-day activities required to keep the practice running smoothly and efficiently.
Core Aspects of Practice Management:
- Patient Scheduling: Effective scheduling ensures optimal use of resources and minimizes patient wait times. It involves managing appointment slots, handling cancellations, and coordinating with other healthcare providers.
- Staff Management: Hiring, training, and managing staff are essential for maintaining high standards of patient care and operational efficiency. This includes managing roles, responsibilities, and performance.
- Financial Management: Practice management involves budgeting, financial planning, and managing expenses. Ensuring profitability while providing quality care requires careful financial oversight and strategic planning.
More posts from rose fox
View posts
Electronic Data Exchange: Streamlining Communication in the Digital Age
rose fox · · In today's interconnected world, the efficient exchange of information is critical for businesses and organizations to thrive. Electronic Data Exchange (EDI) emerges as a cornerstone of modern commerce, revolutionizing how data is transmitted and processed between trading par ...

Navigating the World of Medical Software Development: Innovating Healthcare, One Line of Code at a Time
rose fox · In the intricate landscape of modern healthcare, where precision, efficiency, and accuracy are paramount, the role of healthcare software engineering stands out as a cornerstone of progress. These developers, often working behind the scenes, wield their programming prowess to cre ...
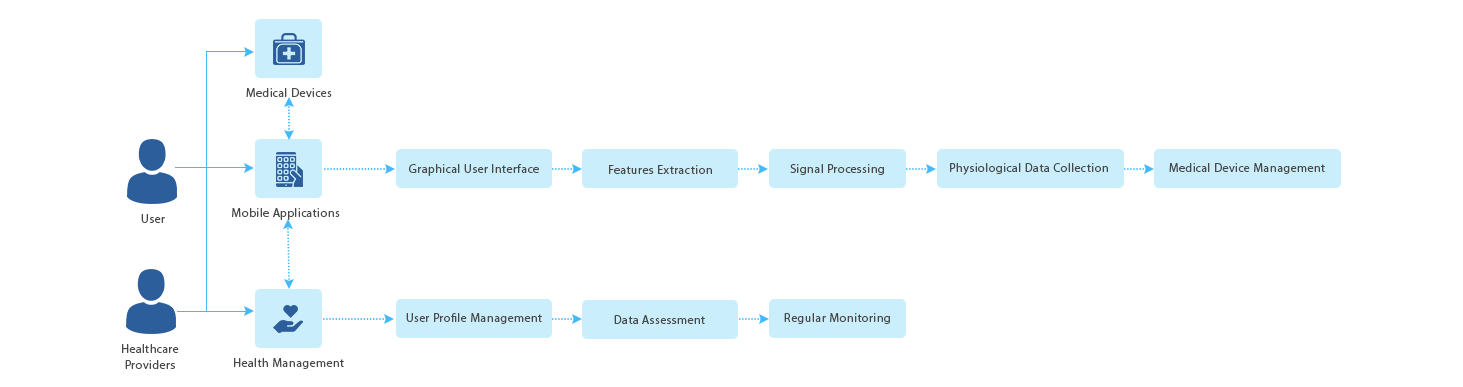
Transforming Healthcare Practice Management through Mobile Health (mHealth)
rose fox · · In recent years, the integration of mobile technology into healthcare, known as mobile health or mHealth, has revolutionized the way medical professionals manage their practices. From patient engagement to administrative tasks, mHealth solutions offer a wide range of benefits ...
You may be interested in these jobs
-
Overview · Join our dynamic healthcare team as a Medical Office Billing Specialist, where your expertise will drive the financial health of our medical practice. In this vital role, you will manage the complete billing cycle, ensuring accurate and timely submission of claims, eff ...
Blue Springs, MO1 week ago
-
+Job summary · Why you'll want to work at nimble ... + · +Responsibilitiesinsurance verification, reviewing submitted claims for accuracy and completenessinvestigating and resolving claim denials by analyzing documentation and using appropriate CPT and ICD-10 codeswork on insuran ...
New Hyde Park2 weeks ago
-
Join a well-established and market-leading brand serving a high-growth end market while gaining valuable experience working closely with Executive leadership. · ...
New Hyde Park1 month ago


Comments